The Living Organ Donor as Patient: Theory and Practice 2021 Original PDF
$14
The Living Organ Donor as Patient: Theory and Practice 2021 Original PDF
When Joseph Murray performed the first successful living kidney donor transplant in 1954, he thought this would be a temporary stopgap. Today, we are no closer to the goal of adequate organ supply without living donors–if anything, the supply-demand ratio is worse. While most research on the ethics of organ transplantation focuses on how to allocate organs as a scarce medical resource, the ethical treatment of organ donors themselves has been relatively neglected. In The Living Organ Donor as Patient: Theory and Practice, Lainie Friedman Ross and J. Richard Thistlethwaite, Jr. argue that living donor organ transplantation can be ethical provided that we treat living solid organ donors as patients in their own right.
Ross and Thistlethwaite develop a five-principle framework to examine some of the attempts to increase living donation. It uses the three principles of the Belmont Report: respect for persons, beneficence, and justice modified to organ transplantation, as well as the principles of vulnerability and special relationships creating special obligations. Their approach requires that the transplant community fully embrace current and prospective living organ donors as patients to whom we have special obligations. Only when living organ donors are regarded as patients in their own right and have a living donor advocate team dedicated to their well-being can the moral limits of living solid organ donation be realized and living donors be given the full respect and care they deserve.
Related Products
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Paramedic Care: Principles and Practice, Volume 1 (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Paramedic Care: Principles and Practice, Volume 2 (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
The Unofficial Guide to Passing OSCEs, 4th edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Uworld USMLE COMLEX Level 1 Qbank, Updated Jan 2023, System- and Subject-wise (PDF)
GENERAL MEDICINE BOOKS
Uworld USMLE Step 1 Qbank, Updated Jan 2023, System- and Subject-wise (PDF)
GENERAL MEDICINE BOOKS
Neinstein’s Adolescent and Young Adult Health Care: A Practical Guide, 7th Edition (EPUB)
GENERAL MEDICINE BOOKS
Medical Pharmacology at a Glance, 9th Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Médecine générale pour le praticien (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Pocket Evidence Based Medicine (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Handbook of Outpatient Medicine, 2nd Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
A Guide to Hospital Administration and Planning (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Nanobiosensors for point-of-care medical diagnostics (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Teaching Evidence-Based Medicine (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
250 Exames De Laboratorio. Prescricao E Interpretação, 10th Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
A Clinician’s Guide to Statistics in Mental Health 2e (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Magill’s Medical Guide, 9th edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
First Aid for the USMLE Step 1 2023, Thirty Third Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Bates’ Guide to Physical Examination and History Taking, 2nd (SAE) (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
UCSF CME COVID-19 for Clinicians: Up-to-the-Minute Advances 2022 (CME VIDEOS)
GENERAL MEDICINE BOOKS
MedStudy 20th Edition Internal Medicine Core Audio Pearls 2022 (Audios)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Anatomia Palpatória Funcional, 2nd Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Ultrassonografia: Revisão, Atualização e Preparação para Provas (EPUB)
GENERAL MEDICINE BOOKS
Uworld COMLEX Level 1 (Step 1 + OMT 1), 3-month Subscription, Full Guarantee (Shared account)
GENERAL MEDICINE BOOKS
Uworld COMLEX Level 1 (Step 1 + OMT 1), 3-month Subscription, 1-month Guarantee (Shared account)
GENERAL MEDICINE BOOKS
Uworld USMLE Step 1, 3-month Subscription, Full Guarantee (Shared account)
GENERAL MEDICINE BOOKS
Uworld USMLE Step 1, 3-month Subscription, 1-month Guarantee (Shared account)
GENERAL MEDICINE BOOKS
ABC of Clinical Reasoning (ABC Series), 2nd Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Radiologia Básica Junior, Carlos Fernando de Mello, 3ª edição (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
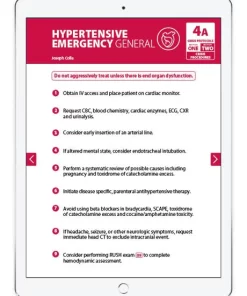
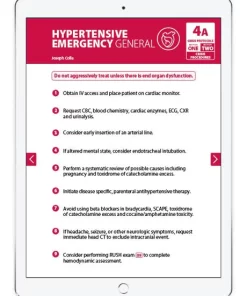
The Resuscitation Crisis Manual (The RCM) eBook (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Goodman and Gilman’s The Pharmacological Basis of Therapeutics, 14th Edition (EPUB)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Bennett & Brachman’s Hospital Infections, 7th Edition (EPUB3)
GENERAL MEDICINE BOOKS
The Washington Manual of Medical Therapeutics, 37th Edition (EPUB3)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Alterazioni idroelettrolitiche e dell’equilibrio acido-base. Diagnosi e terapia (EPUB3)
GENERAL MEDICINE BOOKS
Maximum Malpractice Protection: A Physician’s Complete Guide (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Exam Preparatory Manual For Undergraduates Medicine, 3rd Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
The Washington Manual of Medical Therapeutics, 36th Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Patient-Reported Outcome Measures. Migliorare la cura valorizzando l’esperienza del paziente (EPUB3)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
CURRENT Practice Guidelines in Primary Care 2023 (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Precision Medicine in Clinical Practice (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Essentials of Pathophysiology for Nursing Practice (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Integrative Medicine, 5th edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Diagnóstico físico basado en la evidencia, 5 Edición (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Advanced Practice Provider Skills Made Easy: A Practice Guideline (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Mosby’s® Diagnostic and Laboratory Test Reference, 16th Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
Lubkin’s Chronic Illness: Impact and Intervention, 11th Edition (Original PDF from Publisher)
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
ICD-10-CM/PCS Coding: Theory and Practice, 2023/2024 Edition 2022 Original PDF
GENERAL MEDICINE BOOKS
Introduction to Language Development, 3rd Edition 2022 Original PDF
GENERAL MEDICINE BOOKS
SERS for Point-of-care and Clinical Applications 2022 Original PDF
GENERAL MEDICINE BOOKS
SERS for Point-of-care and Clinical Applications 2022 epub+converted pdf
GENERAL MEDICINE BOOKS
Clinical Decision Making for Improving Prognosis 2022 epub+converted pdf
GENERAL MEDICINE BOOKS
Clinical Decision Making for Improving Prognosis 2022 Original PDF
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Acquiring Medical Language, 2nd Edition 2018 epub+converted pdf
GENERAL MEDICINE BOOKS
Acquiring Medical Language, 3rd Edition 2022 epub+converted pdf
GENERAL MEDICINE BOOKS
GENERAL MEDICINE BOOKS
Phlebotomy: Worktext and Procedures Manual, 5th Edition 2019 Original PDF
GENERAL MEDICINE BOOKS
Uworld ABIM Qbank 2022 (Subject- and System-wise, Updated September 2022) (PDF)
GENERAL MEDICINE BOOKS
Tornado of Life: A Doctor’s Journey through Constraints and Creativity in the ER 2022 Original PDF
GENERAL MEDICINE BOOKS
Pierson and Fairchild’s Principles & Techniques of Patient Care, 7th Edition 2022 Original PDF
GENERAL MEDICINE BOOKS
The Health Care Professional’s Guide to Cultural Competence, 2nd Edition 2022 Original PDF