Pain Review Course
This educational activity allows physicians, registered nurses, and nurse practitioners to earn 45.5 CME/CE credits. This product is the result of a recording of a live meeting providing a comprehensive review of pain management. Pain Review Course with CME (9th Edition) contains valuable information on current pain management practices – including 45 lectures from 10 renowned pain experts.
Pain Review Course with CME (9th Edition)
- AMA PRA Category 1 CME credits™ for physicians
- Class A CE credits for CRNAs
- CBRN credits for registered nurses
- AANP credits for nurse practitioners
- Great preparation for the Pain Board Exam
- Certificates provided via a link
- Post-tests and evaluations required
- Users can print their certificates from their own computer
- Your transcripts are stored to allow you to print additional copies of certificates at any time
Contents
Bernard M. Abrams, M.D.
Clinical Professor of Neurology; University of Missouri School of Medicine; Kansas City, Missouri
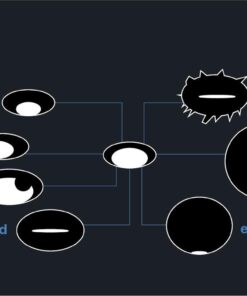
- Neuropathic Pain
- Define the various types of pain.
- Describe various neuropathic pain diagnostic scales and pain intensity scales.
- Identify the underlying mechanism of various pain disorders.
- Central Pain States
- Clarify the differences between central and peripheral neuropathic pain.
- Identify the major types of neuropathic pain.
- List the possible treatments for neuropathic pain.
- Headache
- Explain the anatomical basis of headache syndromes.
- Recognize the types of headache syndromes.
- Identify the available treatments for various headache entities.
- Anatomy of the Upper & Lower Extremities
- Recognize the process of symptomatic, anatomical and etiological diagnosis.
- Discuss the process of referred pain.
- Discern differences between nociceptive and neuropathic pain.
- Extremity Pain
- Identify the anatomical basis of extremity syndromes.
- Discuss the differential diagnosis of extremity syndromes.
- List the available treatments for various extremities.
- Ethical Issues in Pain Management
- Define and describe ethical models and principles.
- Discuss the interface of law (regulatory agencies and rules) and ethics.
- Give examples of ethical challenges in practice.
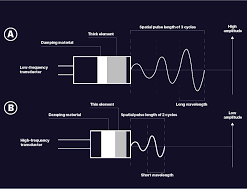
- Clinical Neurophysiology
- Define and describe aspects of neurophysiology.
- Describe physiological basis of tests.
- Review the performance of the exam.
- Enumerate relevant findings in specific conditions.
- Facial Pain
- Express the anatomical basis of facial pain syndromes.
- Recall familiar with the types of facial pain syndromes.
- Associate the available treatments for various facial pain entities.
Kenneth D. Candido, M.D.
Professor of Anesthesiology; Professor and Chairman; Department of Anesthesiology; Advocate Illinois Masonic Medical Center; Chicago, Illinois
- Nociceptive Pain
- Explain the origin of nociceptive pain.
- List common sites of nociceptive pain.
- Trauma Pain Management
- List different trauma events that might present for pain management.
- Review treatment options for pain management in treating these associated injuries.
- Sympathetic Nervous System Related Pain & CRPS
- Review the anatomy and different nerve blocks used for treatment of sympathetic pain.
- Discuss assessing completeness of sympathetic blocks.
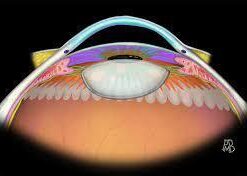
- Head and Neck Blocks
- Review the different nerve blocks for head and neck pain.
- Explain the technique for trigeminal nerve block and gasserian ganglion block in treating facial pain.
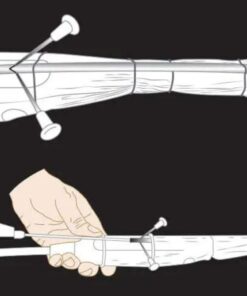
- Brachial Plexus Block Update: State of the Art; PNS vs. US
- Define the structures typically encountered during the performance of ultrasound guided interscalene block of the brachial plexus.
- Explain how ultrasound use has improved the success rates of some, but not all, brachial plexus block approaches.
- Defend the use of ultrasound for providing a reduction in the incidence of ipsilateral hemidiaphragmatic paralysis.
- Lower Extremity Nerve Blocks: PNS vs. US: State of the Art
- Describe the differences in the echogenicity of nerves typically found in the lower extremity, as compared with those above the clavicle.
- Appreciate the rationale for why ultrasound use can lead to local anesthesia sparing effects for sciatic nerve block.
- Clarify the role of adductor canal blocks in lower extremity orthopedic knee procedures.
- Spinal & Epidural Blocks
- Differentiate between and among opioids used perispinally.
- List the pharmacology of adjuvant drugs used spinally.
- Define the risks, benefits and alternatives to spinal drug administration.
Daniel M. Doleys, Ph.D.
- Ethics, Research Design, Elementary Statistics
- Review ethical considerations involved in pain research with humans and animals.
- Review commonly used research designs.
- Outline principles for interpreting research outcomes.
- Review basic statistics and statistical tests.
- “Psychogenic” Pain
- Review the concept of ‘psychogenic pain’.
- Review DSM IV/V diagnoses.
- Discuss the impact of various psychological, mood, and personality factors on pain perception.
- Psychological Assessment of Pain
- Review the relationship between pain mechanisms and the psychological assessment of pain.
- Discuss some of the more common assessment tools/procedures.
- Highlight special concerns with certain patient populations.
- Psychological Treatment of Pain
- Provide an outline of the philosophical basis for psychological therapies.
- Describe some of the more common psychological approaches to the treatment of pain.
- Briefly review outcome data from psychological treatments.
F. Michael Ferrante, M.D., A.B.P.M.
- Painful Medical Conditions
- Describe underlying mechanisms and applications to clinical practice for AIDS.
- Identify the underlying mechanisms of CNS Diseases: Multiple Sclerosis, ALS, Guillain-Barre, etc.
- Explain underlying mechanisms and applications to clinical practice for CV disease/ischemia.
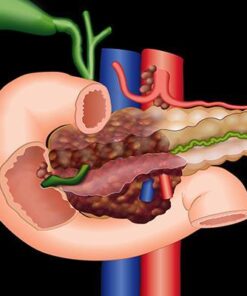
- Describe underlying mechanisms and applications for acute and chronic pancreatitis.
- Identify the underlying mechanisms for rheumatologic diseases.
- Explain underlying mechanisms and applications for Herpes Zoster and Sickle Cell Anemia.
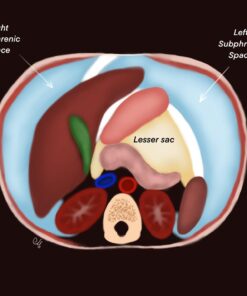
- Anatomy of the Thorax & Abdomen
- Review the anatomy of the thorax.
- Describe the anatomy, physiology, and pharmacology of ANS.
- Apply the anatomy and physiology of Visceral Afferent NS to clinical practice.
- Painful Conditions: Thorax and Abdomen
- Explain the underlying mechanisms and applications to clinical practice for coronary and non-coronary cardiac pain.
- Define the underlying mechanisms and applications to clinical practice for pulmonary embolism.
- Describe the underlying mechanisms and applications to clinical practice for GI pain.
- List the underlying mechanisms and applications to clinical practice for hepatic and biliary pain.
- Explain the underlying mechanisms and applications to clinical practice for pancreatic pain.
- Describe the underlying mechanisms and applications to clinical practice for kidney and ureteral pain.
- Cancer Pain and Symptom Management
- Define the underlying mechanisms and applications for direct tumor involvement/invasion in clinical practice.
- Describe the underlying mechanisms and applications for Neuropathic, Visceral/obstructive, and metastatic cancer in clinical practice.
- List the side effects of diagnosis and therapy for radiation and bone marrow transplantation in clinical practice.
- Explain the underlying mechanisms and applications of psychological reactions to cancer.
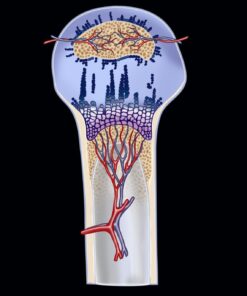
- Pelvic Pain
- Describe the underlying anatomic principles for genesis of pelvic pain.
- Apply anatomic principles to the genesis of chronic painful conditions.
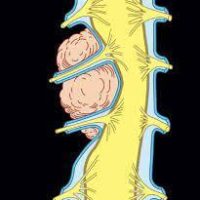
- Anatomy of the Spine
- List the pathological conditions of the vertebrae.
- Describe the disorders of posterior structures.
- Explain the disease of the 5-joint complex (C-Spine) and 3-joint complex (L-Spine).
- Define impingement upon spinal nerve root(s).
- Identify disorders of alignment.
- Describe changes in the size and/or shape of the canal.
- Review disorders of the muscles & fascia.
- Review disorders of postural configuration.
- Radiofrequency Lesioning in Pain Management
- Describe the mechanism underlying production of a lesion for the three major classes of radiofrequency.
- Describe the anatomy of the actual lesion for the three major classes of radiofrequency.
- Describe the innervation of the various joints amenable to radiofrequency.
- Describe the anatomic implications of performance of various radiofrequency procedures.
Benjamin Liu, M.D.
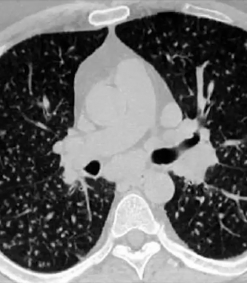
- Imaging of Pain 1 – CT and Plain Films
- Review plain film imaging in the spine.
- Review computed tomography (CT) imaging in the spine.
- Review normal anatomy, degenerative, and nondegenerative back pain pathologies on plain film and CT.
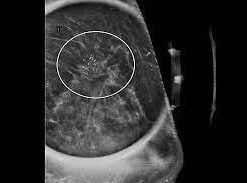
- Imaging of Pain 2 – MRI
- Review basic principles of magnetic resonance imaging (MRI).
- Review normal spinal anatomy, degenerative and nondegenerative causes of back pain on MRI.
- Review standardized degenerative spine nomenclature.
- Imaging of Pain 3 – Bone scan, PET scan, Headaches, Fluoroscopy Radiaiton Safety
- Review basic principles of nuclear medicine bone scan and positron emission tomography (PET), and their role in imaging causes of back pain.
- Review imaging of headache as well as pain diagnosis in other parts of the body.
- Review fluoroscopy and radiation safety in the performance of interventional spine procedures.
Ameet S. Nagpal, M.D.
- Function, Impairment, Disability, & Handicap
- Define function and functionality and discuss related measurement scales.
- Define impairment according to varied sources and discuss related measurement scales.
- Define disability (activity limitation) according to varied sources and discuss related measurement scales.
- Define handicap (participation restriction) according to varied sources.
- Briefly discuss physical medicine treatment options related to activity limitations and participation restrictions.
- Trigger Points & Peripheral Joint Injections
- Define the terms tender point and trigger point and identify the treatment solutions for both.
- Describe the indications for, contraindications of, and appropriate exercise regimens for peripheral injections in the shoulder, elbow, and wrist/hand.
- Describe the indications for, contraindications of, and appropriate exercise regimens for peripheral injections in the hip, knee, and ankle/foot.
- Rehabilitation Medicine Approach to Chronic Pain Management
- Describe the role of the heat and cold in the treatment of chronic pain.
- Describe the role of the Manual (osteopathic) manipulation and mobilization in the treatment of chronic pain.
- Describe the role of electricity; massage; traction; splinting/orthotic devices; and exercise in the treatment of chronic pain.
Maunak Rana, M.D.
- Opioids, REMS, Prescription Writing
- Review the pharmacology and physiology of opioid medications.
- Review the REMS program – history and background.
- Discuss strategies to mitigate problematic opioid use.
- Review prescription writing of opioids.
- NSAIDs, Muscle Relaxants
- Identify the classification of opioids compounds.
- Explain the pharmacology of pain transmission and modulation.
- Describe the pharmacokinetic and pharmacodynamics properties of NSAIDs and muscle relaxants and identify potential adverse side effects, drug interactions, and indications/contraindications for them.
- Assess opioids and an optional treatment of pain.
- Steroids, Anti-Depressants, and Anti-Convulsants
- Review classification of anti-depressants and anti-convulsants and their use in pain states.
- Identify potential drug interactions among anti-depressants, anti-convulsants, steroids and other pharmaceutical pain treatment options.
- Review the properties of steroids as they pertain to treatment of painful conditions.
- Complementary and Alternative Medicine
- Discuss alternative medical systems and therapies describing the prevalence and evidence base for each.
- Review potential implications, costs and side effects of alternative therapies.
- Identify complementary therapies for treatment of pain.
- Hospice and Pain Management in War and Underserved Areas
- Review the concept of palliative medicine and hospice care.
- Discuss pain management in Hospice patients.
- Discuss pain management in underserved populations.
- Review pain management and functional rehabilitation in military environments.
- Pediatric Pain Management
- Review physiologic differences between pediatric and adult patients.
- Review Pharmaco-kinetic and Pharmacodynamic issues in pediatric patients.
- Present the assessment of pediatric pain patients.
- Review interventional and non-interventional therapies for pediatric pain patients.
- Geriatric Pain Management
- Review the physiologic changes in Geriatric patients and associated health issues.
- Review the Pharmaco-kinetic and Pharmacodynamic issues in Geriatric Patients.
- Present the assessment of Geriatric pain patients.
- Review interventional and non-interventional therapies for geriatric patients.
Meghan Rodes, M.D.
- Obstetric Pain Management
- Review innervation of the uterus and birth canal.
- Discuss analgesic approaches for labor and delivery.
- Special Concerns in Pregnancy and Lactation in the Management of Pain
- Discuss the factors determining the placental transfer of medications to the fetus.
- Examine the factors involved in the transfer of medications to breast milk.
- Review the effects of medications on the fetus and neonate.
- Review the effects of radiation exposure.
- Discuss management of common pain conditions in pregnancy.
- Overview of Neurosurgical Invasive Techniques
- Review neurosurgical approaches to pain relief in the pain patient.
- Give a brief overview of the role of pain procedures in neurosurgery.
- Provide indications for neurosurgical pain procedures.
- Discectomy and Minimally Invasive Spine Surgery
- Review indications, contraindications and risks of invasive spine surgery.
- Discuss patient presentation with lumbar pain syndromes.
- Discuss indications and options for surgery.
- Discuss indications, results and complications of kyphoplasty and vertebroplasty.
- Neuromodulation
- Describe differing types of neuromodulation procedures.
- Explain and apply: Indications; Techniques of implantation; Use of common medications/programming and algorithms; Potential problems and complications.
Oren Sagher, M.
Tony L. Yaksh, Ph.D.
- Biology of Pain Processing
- Review basic anatomy of the i) primary afferent; ii) spinal dorsal horn; iii) ascending projection pathways; iv) brainstem-thalamocortical systems involved in pain processing.
- Review response properties of primary afferents and dorsal horn neurons that encode nociceptive information.
- Define systems that underlie the sensory-discriminative and affective-motivational components of the pain experience.
- Post Tissue Injury Pain
- Response of primary afferent exposed to inflammation.
- Spinal properties mediating 1st and 2nd hyperalgesia.
- Systems/Pharmacology regulating dorsal horn input/output function in normal and post tissue injury pain states.
- Discuss changes in neural processing that lead from an acute (transient) pain state to a persistent pain state.
- Post Nerve Injury Pain
- Response of afferent/DRG and spinal cord to physical and chemical injury of peripheral nerve.
- Review mechanisms whereby peripheral nerve injury leads to on going pain sensations (e.g. dysesthesias).
- Review changes in spinal processing that underlie development of pain secondary to low threshold mechanical stimulation. (e.g. tactile allodynia).
- Acute to Chronic Pain
- Consider the acute to chronic pain phenotype e.g. transition of an acute injury/inflammatory state to a chronic post inflammatory pain state.
- Review current thinking on the mechanism that underlie the acute to chronic pain transition.
- Understand the role of innate immunity in the chronic pain phenotype.
Only logged in customers who have purchased this product may leave a review.
Related Products
PLASTIC & RECONSTRUCTIVE SURGERY
Mohs Micrographic Surgery: From Layers to Reconstruction Original PDF and Videos
PLASTIC & RECONSTRUCTIVE SURGERY
Global Rhinoplasty: A Multicultural Approach Original PDF and Videos
GASTROINTESTINAL SURGERY
Blumgart’s Video Atlas: Liver, Biliary & Pancreatic Surgery 2nd Edition PDF Original & Video
DERMATOLOGY
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Assessment and Effective Treatment of Alcohol and Substance Abuse Disorders 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
2020 Mayo Clinic “Teach the Teachers” Elbow Course – Forging the Future
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
2021 AAN Advanced Practice Provider Neurology Education Series
Video + Ebooks Other
Video + Ebooks Other
Third Edition: Modern Surgical Pathology Through the Expert Eyes of APSS-USCAP 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Venous Disease: Exploration of Advances, Challenges, and Future Directions 2021
Video + Ebooks Other
Video + Ebooks Other
SAR Disease-Focused Panels: Cancer Imaging and Reporting Guidelines 2021
Video + Ebooks Other
Video + Ebooks Other
ARRS Abdominal MRI: Practical Applications and Advanced Imaging Techniques 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Baylor College of Medicine Annual GI and Hepatology Board Review Course 2021
Video + Ebooks Other
Imaging Mastery Series: Regulatory/Standards of Care in Breast Imaging 2021
Video + Ebooks Other
2019 Annual Meeting Long Course – Common Problems in Dermatopathology
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
EMERGENCY MEDICINE BOOKS
Video + Ebooks Other
APA (American Psychiatric Association) Annual Meeting On Demand 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
40th ISICEM International Symposium on Intensive Care & Emergency Medicine 2021
Video + Ebooks Other
Video + Ebooks Other
USCAP The Old and The New: A Comprehensive Approach to the GI Tract 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Imaging Mastery Series: Pathology of the Oral Cavity and Oropharynx 2020
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Hematopathology Tasting Menu: A Sampling of Delightful Diagnostic Challenges 2021
Video + Ebooks Other
Gynecologic Pathology: Navigating Histologic Mimics and Other Diagnostic Pitfalls 2021
Video + Ebooks Other
Video + Ebooks Other
Culinary Health Education Fundamentals (CHEF) Coaching—The Basics
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
MRI Mastery Series: Intradural Extramedullary Lesions (IDEM) 2020
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Imaging Mastery Series: Fetal Heart and Great Vessel Evaluation 2021
Video + Ebooks Other
Video + Ebooks Other
Imaging Mastery Series: Image-Guided Abscess Drainage in Interventional Radiology 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Specialty Review in Pediatric Cardiology Virtual Course 2021
Video + Ebooks Other
PERIPHERAL NERVE ULTRASOUND: INTERVENTIONAL & NEUROLOGY APPLICATIONS 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
The American Clinical Neurophysiology Society (ACNS) Virtual Fall Courses & Symposium 2021
Video + Ebooks Other
Fundamentals of Musculoskeletal Ultrasound Course — San Diego 2021




















































Reviews
There are no reviews yet.