Anesthesiology Review Course
This educational activity allows anesthesiologists to earn 40.0 CME/CE credits. This product is the result of a recording of a live meeting providing a comprehensive review of the specialty of anesthesiology. Anesthesiology Review Course with CME (8th Edition) contains valuable information on current anesthesiology practices – including 40 complete lectures from 13 renowned anesthesiology experts.
Anesthesiology Review Course with CME (8th Edition)
- AMA PRA Category 1 CME credits™ for physicians
- Great preparation for a Board Exam
- Certificates provided via a link
- Post-tests and evaluations required
- Users can print their certificates from their own computer
- Your transcripts are stored to allow you to print additional copies of certificates at any time
Contents
Jerrold Levy, M.D.
Professor of Anesthesiology; Duke University School of Medicine; Durham, NC
- Anaphylaxis, Allergy and Adverse Drug Reactions
- Review the different adverse drugs reactions and life threatening anaphylactic and allergic reactions a clinician may encounter.
- Understand different mechanisms of anaphylaxis and discuss agents most often responsible for reactions including drugs, blood products, and environmental agents including latex.
- Discuss therapeutic approaches to the treatment and prevention of anaphylactic reactions and cardiopulmonary dysfunction that occurs.
- Anticoagulant to Procoagulant Therapies: Understanding the Coagulation Cocktails
- Summarize the pharmacologic therapies that affect hemostasis and the coagulation system.
- Review the role of perioperatively acquired disorders of coagulation and implications for bleeding.
- Identify the new anticoagulation agents recently approved and their perioperative management.
- Discuss pharmacologic strategies for decreasing postoperative bleeding, reducing transfusion coagulopathy, and reversing anticoagulation.
- New Concepts in the Treatment and Prevention of Bleeding
- Summarize the mechanisms and etiologies of perioperative disorders of coagulation.
- Identify patients undergoing surgery who are at risk for acquired coagulopathy and bleeding.
- Discuss strategies for decreasing post-operative bleeding and reducing transfusion coagulopathy including blood products and pharmacologic therapies.
James G. Ramsay, M.D.
Professor of Anesthesiology; University of California San Francisco; San Francisco, CA
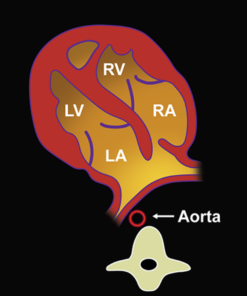
- Preoperative Cardiac Evaluation: AHA Guidelines and Beyond
- Be able to apply recent published guidelines in managing preoperative cardiac evaluation.
- Be able to compare the procedure intensive approach of evaluation vs the biomarker intensive approach.
- Be able to compare published risk indices Revised Cardiac Risk Index (RCRI) and American College of Surgeons National Quality Initiative (ACS-NSQUIP) to evaluate the risk of an adverse perioperative cardiac event.
- Be able to recommend a rational approach for evaluation in the patient with known coronary artery disease.
- Management of the Cardiac Patient for Noncardiac Surgery
- Be able to describe the preoperative evaluation of a patient with a cardiac murmur.
- Be able to interpret the preoperative evaluation of aortic stenosis and the implications for perioperative management.
- Be able to recommend an anesthetic management plan for the patient with severe aortic stenosis undergoing noncardiac surgery.
- Be able to compare the outcomes of patients undergoing percutaneous aortic valve replacement vs. open surgical replacement.
- Pacemakers, ICDs and VADs, (“oh no!”)
- Be able to evaluate whether a patient has a pacemaker vs implantable cardiac defibrillator (ICD).
- Be able to appropriately manage a pacemaker/ ICD in a patient who is pacemaker dependent.
- Be able to recommend intraoperative management of electrosurgical devices and other devices which may affect the function of a pacemaker or ICD.
- Be able to evaluate the need for invasive arterial pressure monitoring in a patient with a ventricular assist deivce.
Pamela Flood, M.D.
Professor of Anesthesiology; Professor of Perioperative and Pain Medicine; Stanford School of Medicine; Stanford University; Standford, CA
- Anesthetic Considerations for Patients with Chronic Pain: How to Make Them Wake Up Happy
- Understand the psychological needs of patients with chronic pain who require procedures.
- Understand the pharmacological needs of patients on chronic opioids.
- Devise a plan for a chronic pain patient who requires an intervention at your hospital.
- Pre-eclampsia and Eclampsia
- To review recent changes in nomenclature for hypertensive disease of pregnancy and its clinical rational.
- To review management of the patient with hypertensive disease of pregnancy.
- Considerations for Labor Analgesia
- Describe the physiology of labor pain.
- Devise a plan for the management of labor pain.
- Explain upon the technique for epidural placement.
- Explain the risks of neuraxial labor analgesia.
- Anesthesia for Cesarean Section
- Understand the anesthetic requirements for anesthesia for cesarean delivery.
- Devise a plan for the parturient who requires urgent cesarean delivery.
- Explain the concern for general anesthesia during cesarean delivery.
- Explain why phenylephrine is preferred for the treatment of hypotension.
James B. Eisenkraft, M.D.
Professor of Anesthesiology; Mount Sinai School of Medicine; New York, NY
- Understanding the Anesthesia Machine
- Describe how medical gases are stored and delivered to the anesthesia machine.
- Describe how the gases flow through the machine to the common gas outlet and the components of the pathways.
- Anesthesia Breathing Systems, Ventilators and Waste Gas Scavenging Systems
- Describe the structure and function of commonly used breathing systems.
- Describe the function of anesthesia ventilators.
- Cite the structure and function of waste gas scavenging systems.
- Hazards of the Anesthesia Workstation
- Describe critical incidents and adverse outcomes related to the use of anesthesia delivery systems.
- Describe strategies to improve the safe use of anesthesia delivery systems.
Benjamin J. Wallisch, D.O.
Associate Professor/Department of Anesthesiology; University of Texas School of Medicine at San Antonio; San Antonio, TX
- Anesthesia for the Patient with Diabetes Mellitus
- Describe the pathophysiology of diabetes mellitus and its subtypes.
- Combining this knowledge with an overview of current treatments for diabetes, attendees will be able to design an anesthetic plan for specific diabetic patients who frequently present to the operating room.
- Everyday Endocrine Disease and Anesthesia
- Describe the pathophysiology and anesthesia implications of important endocrine disorders including thyroid dysfunction, parathyroid disfunction, pituitary disease, and diseases of the adrenal gland.
- Identify and treat common surgical and anesthesia complications associated with procedures involving the endocrine system.
John C. Rowlingson, M.D.
Professor of Anesthesiology and Director of Acute Pain Management Services; University of Virginia Health System; Charlottesville, VA
- Acute Pain Pathophysiology for the Clinician
- Review the anatomy and physiology of the pain transmission system.
- Discuss the changes the occur in the peripheral and central nervous systems.
- Relate the altercations in the pain projection system with clinical events.
- Clinical Use of and Concerns About Opioid Use in Pain Management
- Present a review of basic opioid pharmacology.
- Discuss issues relevant to the clinical use of opioids in patients with acute, chronic and cancer pain.
- Present the side/ adverse effects and the consequences of chronic opioid use and their impact on contemporary outcome assessment.
- Contemporary Acute Pain Management: Aiming to Improve Clinical Outcome
- Describe the rationale for treatment options based upon pain physiology.
- Discuss contemporary pain management modalities.
- Discuss the need to modernize our view of outcome assessment beyond VAS system.
John C. Drummond, M.D., FRCP(C)
Professor of Anesthesiology; University of California at San Diego; Staff Anesthesiologist; VA Medical Center; San Diego, CA
- Neuroanesthesia: Physiology and Pharmacology Relevant to Critical Situations
- A systematic approach to the manipulation of the volume of the intracranial contents.
- An understanding of the physiology of the effect of PaCO2 on cerebral blood flow.
- An understanding of the relevance of CBF-CMR coupling to the CBF effects of anesthetic agents.
- An understanding of the very variable, pathology dependent effect of volatile agents on CBF.
- An understanding of the effects of intravenous anesthetic agents on cerebral blood flow and metabolism.
- An understanding of the relative clinical effects of mannitol and hypertonic saline.
- Describe the cerebral protective potential of intravenous agents and of moderate hypothermia.
- Neuroanesthesia: Situation-Specific Considerations (Head Injury, Aneurysm, Posterior Fossa)
- The principles that guide intraoperative physiologic management targets including cerebral perfusion pressure, carbon dioxide tension and temperature in the TBI patient.
- The principles that govern management of hyperglycemia in the brain injured patient (and how they differ from other critical care patients).
- The principles that govern blood pressure management in the patient who has recently sustained a subarachnoid hemorrhage.
- The anesthetic considerations for interventional management (coiling) of intracranial aneurysms.
- The status of induced hypothermia in the management of aneurysm clipping.
- The standard of care for monitoring for the detection of venous air embolism.
- The hemodynamic effects of manipulation of posterior fossa structures.
- The etiology/physiology of tension pneumocephalus.
- The causes and consequences of the macroglossia phenomenon.
- Blood Pressure and the Brain: How Low Can You Go?
- Both the numeric value of the average lower limit of cerebral blood flow (CBF) autoregulation and its inter-individual variability.
- The CBF (and BP) thresholds at which CNS dysfunction and then injury are likely to occur.
- The concept of the CNS blood flow reserve and of the physiologic phenomena that reduce that reserve in some patients.
- Are You Confused About Delirium (and its causation, prevention and treatment)?
- The criteria for a diagnosis of delirium.
- The clinical characteristics and events that are recognized as, respectively, predisposing to and precipitating delirium.
- The pharmacologic do’s and don’ts relevant to the prevention and treatment of delirium.
- The non-pharmacologic methods for the prevention of nosocomial delirium.
- The relationship between depth of anesthesia and the occurrence of delirium.
Kenneth D. Candido, M.D.
Professor of Anesthesiology; Professor and Chairman; Department of Anesthesiology; Advocate Illinois Masonic Medical Center; Chicago, IL
- Ultrasound Use for Upper Extremity Surgery: Has It Made a Difference?
- Explain the distances from the skin to the neural foramen and spinal cord at the level at C6 in adults.
- Describe the utility of the respective approaches to brachial plexus block for upper extremity surgery, including the indications and contraindications of each technique.
- Explain the relative complications of brachial plexus block, including the incidence(s) and mechanisms underlying the common ones.
- List the appropriate indications for ultrasound guidance in brachial block anesthesia.
- Describe the alternatives to brachial plexus block for upper limb surgery.
- Ultrasound Use for Lower Extremity Surgery: What Have We Learned?
- Explain the relationship of the two component nerves, tibial and common peroneal, one to the other, as well as the common techniques of providing complete sciatic nerve blockade.
- Identify the most appropriate lower extremity regional technique for the intended surgery.
- Provide the rational for selecting one type of evoked motor response over another when performing lower extremity block(s) using peripheral nerve simulator assistance.
- Describe the most appropriate uses of ultrasound guidance for lower extremity block.
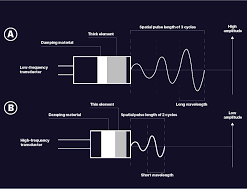
- Basics of Ultrasonography: Science and Knobs
- Describe the theoretical framework for ultrasound anatomic imaging.
- Describe visual elements that indicate the proper placement of local anesthetic agents.
J. Matthew Aldrich, M.D.
- Ventilating the (potential) ICU Patient to, from, and in the OR
- Describe the key methods for mechanical ventilation in the ICU and the operating room.
- Develop a plan for mechanical ventilation in the operating room for patients with and at risk for lung injury.
- Sepsis: What the Anesthesiologist Needs to Know
- Summarize the randomized control trials of early goal directed therapy for septic shock.
- Integrate key components of the Surviving Sepsis Campaign’s guideline into an anesthetic plan, with particular focus on initial resuscitation techniques and hemodynamic support.
- Anesthesia for the Patient Undergoing Endovascular Aortic Repair
- Describe the risks for cardiac, pulmonary, renal and spinal cord complications.
- Formulate an anesthetic plan for an endovascular thoraco-abdominal aortic repair, emphasizing intraoperative hemodynamic monitoring and perioperative spinal cord protection.
Francis Chung, M.D.
- Morbidly Obese Patients: A Clinical Challenge
- To evaluate the co-morbidities of morbidly obese patients and patients with obesity hypoventilation syndrome.
- To appraise the preoperative assessment, intraoperative and postoperative management of these patients.
- Obstructive Sleep Apnea: What the Anesthesia Provider Should Know?
- Evaluate the evidence of postoperative complications in patients with obstructive sleep apnea.
- Identify patients with undiagnosed obstructive sleep apnea.
- Appraise the efficacy of preoperative and postoperative CPAP and BiPAP.
- Review management of these patients as part of the Perioperative Surgical Home.
- Enhanced Recovery from Surgery
- To review the evidence to support enhanced recovery after surgery.
- To appraise the useful recommendations that can be adopted for enhanced recovery after surgery.
- To identify the implementation strategies to facilitate the process of enhanced recovery after surgery.
Ronald B. Easley, M.D.
- Anesthetic Management of Common Pediatric Emergencies
- Preparedness for a Pediatric Emergency.
- Common Pediatric Emergencies and Anesthesia.
- Adjunct Tools – Pedi-Crisis Checklist.
- Anesthesia for Common Diagnostic and Therapeutic Radiologic Procedures in Children
- Identify all key critical patient safety risk issues in pediatric sedation and anesthesia in radiology.
- Describe key personnel and system components necessary for delivery of safe pediatric sedation and anesthesia, and explain the role of each.
- Propose a “best practice” model for anesthesia in radiology, and analyze the differences between this and the existing model at the participant’s institution.
- Perioperative Management of the Child with Respiratory Disease
- Review the basic principles of pulmonary physiology (child vs. adult).
- Review common pediatric pulmonary diseases and their pathophysiology.
- Be able to give rational pre-, intra- and post-anesthetic considerations in caring for patients with these diseases.
Steven L. Shafer, M.D.
- Pharmacokinetics and Pharmacodynamics: Basic Principles
- Understand the concepts of volume, clearance, and effect site
- Understand that one compartment models do not describe intravenous anesthetics, and may lead to incorrect conclusions.
- Understand how time to peak effect and context-sensitive half time can improve drug administration.
- Opioids: Basic and Clinical Pharmacology
- Understand the time course of opioid onset following intravenous bolus
- Understand the distinguishing characteristics of morphine, hydromorphone, fentanyl, alfentanil, sufentanil, and remifentanil
- Understand how blood-brain equilibration has more influence is a greater determinant of onset and offset than plasma pharmacokinetics
- Sedative Hypnotics: Basic and Clinical Pharmacology
- The time course of propofol and midazolam onset and offset
- The influence of age on propofol and midazolam pharmacokinetics
- How to administer propofol for long cases and ensure rapid recovery
Peter D. Slinger, M.D.
- Anesthesia for Patient with Severe Lung Disease
- Explain the factors involved in carbon dioxide retention in COPD
- Review the physiology of intraoperative dynamic hyperinflation
- Develop a plan for perioperative management of a patient with pulmonary hypertension for non-cardiac surgery.
- Management of One-Lung Ventilation
- Understand recent advances in the available options for lung isolation in thoracic surgery.
- To discuss the pros and cons of bronchial blockers vs. double-lumen tubes for lung isolation
- Develop a protocol to deal with lung isolation in patients with difficult airways.
- Develop an approach to the prevention and treatment of hypoxemia during one-lung ventilation.
- Anterior Mediastinal Masses and Lower airway Problems
- Review the pre-anesthetic assessment of a patient with an anterior mediastinal mass.
- Develop a plan for perioperative management of a patient with an anterior mediastinal mass.
- Identify the anesthetic considerations for rigid bronchoscopy
- Develop a strategy to manage patients with lower airway complications
Only logged in customers who have purchased this product may leave a review.
Related Products
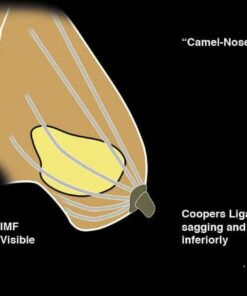
PLASTIC & RECONSTRUCTIVE SURGERY
Mohs Micrographic Surgery: From Layers to Reconstruction Original PDF and Videos
PLASTIC & RECONSTRUCTIVE SURGERY
Global Rhinoplasty: A Multicultural Approach Original PDF and Videos
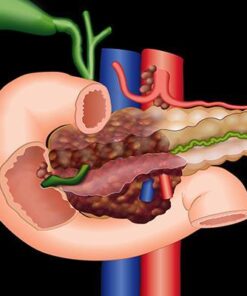
GASTROINTESTINAL SURGERY
Blumgart’s Video Atlas: Liver, Biliary & Pancreatic Surgery 2nd Edition PDF Original & Video
DERMATOLOGY
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Assessment and Effective Treatment of Alcohol and Substance Abuse Disorders 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
2020 Mayo Clinic “Teach the Teachers” Elbow Course – Forging the Future
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
2021 AAN Advanced Practice Provider Neurology Education Series
Video + Ebooks Other
Video + Ebooks Other
Third Edition: Modern Surgical Pathology Through the Expert Eyes of APSS-USCAP 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Venous Disease: Exploration of Advances, Challenges, and Future Directions 2021
Video + Ebooks Other
Video + Ebooks Other
SAR Disease-Focused Panels: Cancer Imaging and Reporting Guidelines 2021
Video + Ebooks Other
Video + Ebooks Other
ARRS Abdominal MRI: Practical Applications and Advanced Imaging Techniques 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Baylor College of Medicine Annual GI and Hepatology Board Review Course 2021
Video + Ebooks Other
Imaging Mastery Series: Regulatory/Standards of Care in Breast Imaging 2021
Video + Ebooks Other
2019 Annual Meeting Long Course – Common Problems in Dermatopathology
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
EMERGENCY MEDICINE BOOKS
Video + Ebooks Other
APA (American Psychiatric Association) Annual Meeting On Demand 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
40th ISICEM International Symposium on Intensive Care & Emergency Medicine 2021
Video + Ebooks Other
Video + Ebooks Other
USCAP The Old and The New: A Comprehensive Approach to the GI Tract 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Imaging Mastery Series: Pathology of the Oral Cavity and Oropharynx 2020
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
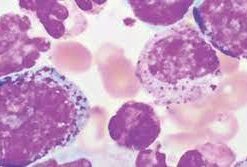
Hematopathology Tasting Menu: A Sampling of Delightful Diagnostic Challenges 2021
Video + Ebooks Other
Gynecologic Pathology: Navigating Histologic Mimics and Other Diagnostic Pitfalls 2021
Video + Ebooks Other
Video + Ebooks Other
Culinary Health Education Fundamentals (CHEF) Coaching—The Basics
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
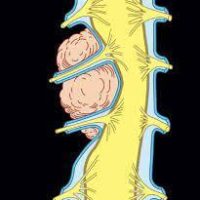
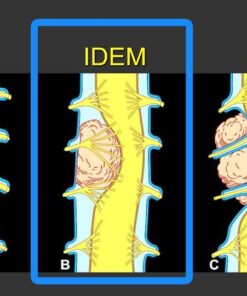
MRI Mastery Series: Intradural Extramedullary Lesions (IDEM) 2020
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Imaging Mastery Series: Fetal Heart and Great Vessel Evaluation 2021
Video + Ebooks Other
Video + Ebooks Other
Imaging Mastery Series: Image-Guided Abscess Drainage in Interventional Radiology 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
Specialty Review in Pediatric Cardiology Virtual Course 2021
Video + Ebooks Other
PERIPHERAL NERVE ULTRASOUND: INTERVENTIONAL & NEUROLOGY APPLICATIONS 2021
Video + Ebooks Other
Video + Ebooks Other
Video + Ebooks Other
The American Clinical Neurophysiology Society (ACNS) Virtual Fall Courses & Symposium 2021
Video + Ebooks Other
Fundamentals of Musculoskeletal Ultrasound Course — San Diego 2021




















































Reviews
There are no reviews yet.